Watch a short video that describes what a congenital diaphragmatic hernia is and how we treat it at Primary Children's Hospital in Salt Lake City, Utah
Understanding Congenital Diaphragmatic Hernia (CDH)?

What is a CDH?
A CDH is an abnormality in the diaphragm which leads to an opening or hole between the abdomen and the chest. This allows the contents of the abdomen to move into the chest which can include: stomach, small intestine, spleen, liver, and/or kidneys. The presence of these organs in the chest prevents the lungs from developing properly, resulting in pulmonary hypoplasia (or too small of lungs). Additionally, the blood vessels in the lungs become overly muscular leading to hyperreactivity and increased blood pressure in the lungs, called pulmonary hypertension. This pressure makes blood flow difficult through the lungs and makes it difficult to get the right amount of oxygen. The resulting pulmonary hypoplasia and pulmonary hypertension inhibit the lungs from working correctly and are what make the child sick immediately following birth.
- Occurs in 1 in 3,000 live births
- Most commonly happens on the left side
- 30% are associated with other abnormalities
- Usually found on screening ultrasound

Fetal Center: The first step in CDH care
Multidisciplinary Evaluation: meet with MFM specialist, pediatric surgeon, neonatologist, and other experts who will care for your baby
Comprehensive Imaging: detailed ultrasounds and other tests when indicated to assess your baby's condition and help plan treatment
Coordinated Delivery Planning: our team works to ensure your baby receives immediate specialized care at birth

How is a CDH evaluated?
The CDH is typically found during a routine pregnancy ultrasound around 20 weeks of gestation. After the defect is seen, we recommend that you have a series of follow-up studies including:
- A comprehensive ultrasound will give us more detail about the other body structures that may be affected.
- A fetal MRI gives us advanced images of your baby including the position of the liver and the observed-to-expected fetal total lung volume ratio (MRI O/E). This information will help us determine how much your baby will be affected by the CDH after delivery. It also gives detailed information about the rest of the child.
- A fetal echocardiogram is an ultrasound of the baby’s heart that is performed by a pediatric cardiologist. This test is recommended to look at the heart structure and function.
- An underlying syndrome is present in approximately 10% of cases and you will meet with a genetic counselor who can give you more information regarding screening tests.
All of this information will help the fetal team give you the most accurate information so that patients and their families can make the best possible decision about treatment.
(pic: fetal MRI with calculations to obtain O/E ratio)

How does a CDH affect your baby?
A CDH can cause mild to very severe problems with lung and heart function depending on the severity of the pulmonary hypoplasia and pulmonary hypertension. The location and severity of the CDH will play a part in how your baby will be affected. There are several prenatal prediction factors that will help us anticipate how severe the child will be affected following delivery:
Liver position: The position of the liver in the chest or abdomen can be determined on both fetal ultrasound or fetal MRI:
- Intrathoracic (liver up): poor prognosis, higher risk of need for ECMO (~15%), lower overall survival (~70%)
- Intraabdominal (liver down): better prognosis, lower risk of need for ECMO (~3%), higher overall survival (~95%)
Ultrasound Lung-to-Head Ratio (LHR): This ratio is obtained during the fetal ultrasound. The area of the lung on the opposite side of the CDH is measured at the level of the heart and then divided by the circumference of the head.
- LHR < 1: poor prognosis, higher risk of need for ECMO and lower overall survival
- LHR > 1.4: better prognosis, lower risk of need for ECMO with higher overall survival

MRI observed-to-expected Total Fetal Lung Volume (MRI O/E): This number is obtained following a fetal MRI, where the radiologist measures the volume of both lungs (observed) and then divides them by what the volume should be (expected) at that gestation in a child without a CDH. The results are divided into 4 risk categories:
- > 35%: Mild severity with the lowest risk for ECMO (2%), highest overall survival (96%), and average hospital course of 1 month
- 25 – 35%: Moderate severity with lower need for ECMO (13%), overall higher survival (90%) and average hospital length of stay of 2 months
- < 15 - 24.9%: Severe CDH with highest risk of ECMO (29%), lower rate of survival (80%) with an average hospital stay of 3 months
- < 15%: Very severe CDH with high need for ECMO (23%) with the lowest rate of survival (23%) and overall longest hospital course (average 4 months)
Based on these prenatal predictors, the fetal team can discussed the anticipated severity of your child’s disease and what to expect after delivery.
(pic: fetal MRI demonstrating left sided CDH)
Our Utah Experience: Personalized Care Based on MRI O/E





How is CDH managed during pregnancy?
Once a diagnosis of CDH is made, we recommend early evaluation at the Grant Scott Bonham Fetal Center, including a fetal ultrasound to determine liver position and LHR. This will allow us to determine whether your baby qualifies for fetal therapy.
Although not currently offered at our Fetal Center, the Fetoscopic Endoluminal Tracheal Occlusion (FETO) trial is underway at select centers across the country. In this initial evaluation, we can discuss the criteria for the trial and whether referral to one of these centers is appropriate. If so, we will help arrange contact at one of these centers for further evaluation.
You should be closely monitored during your pregnancy. Our multi-disciplinary team will review your imaging and give you information about the CDH, give recommendations on management of your pregnancy, and help you meet with the pediatric specialists that will take care of your baby after delivery.

How is a child with CDH managed during and after delivery?
Babies with CDH should be delivered at our center where a neonatal intensive care unit (NICU) is available that specializes in the care of CDH infants and where a pediatric surgeon can immediately evaluate your child. The neonatologist is a specially trained pediatrician that will manage your baby’s medications, feeding, and daily needs while in the NICU. Once the child is born, a neonatologist will evaluate the baby and make sure the heart and lungs are working appropriately.
At Primary Children's Hospital we have unique way of caring for these children which has led to us being #1 in outcomes according to Children's Hospital Association Data. In the first few days of life we allow the child to stabilize and let their little lungs get used to working without too much stress by:
- Weaning oxygen according to heart function
- Starting sedation early to keep the child calm and pain free
- Providing lower initial lung pressures on the ventilator
- Waiting over 1 day to perform the initial heart ultrasound
- Limit the use of medications that affect blood pressure (iNO and inotropes)
A tube placed through the mouth (oral gastric or OG) all the way to the stomach. This tube will suck out any fluid with in the stomach to prevent your baby from choking or breathing stomach contents into the lungs and to prevent the intestines from becoming too dilated with air.
Your baby will receive fluids and antibiotics through a special IV called a PICC line, initially through the umbilical cord, then placed in one of the limbs. Because the child will not be initially allowed to eat, they will also receive nutrition through the PICC line called TPN, or total parenteral nutrition. TPN contains protein, fat, sugar, vitamins, and minerals and will meet all your baby’s nutritional needs. Medications will also be given to assist with the function of the lungs and heart.
(pic: child undergoing treatment for severe CDH)

When will surgery happen to repair the CDH?
Although surgical repair of the CDH is needed, the initial priority is to support the function of the heart and lungs. The surgical procedure is delayed until the child is felt to be stable enough to undergo repair. In some cases, the CDH is so severe that the lungs and heart cannot provide the necessary functions to survive. The lungs and heart may need additional support. In this case, Extracorporeal Membrane Oxygenation (ECMO) may be an option. This is a machine which functions like the heart and lungs. It can provide support for just the lungs (VV-ECMO) or both the lungs and heart (VA-ECMO). It acts like a “heart-lung bypass” to let the baby’s heart and lungs rest, heal, and develop. This support is offered at Primary Children’s Hospital, who has an ECMO team and has years of experience caring for these critically ill children. Approximately 12% of infants we treat with CDH will require ECMO support.

Are there different types of repair?
Once your child is stable enough to undergo surgery, the CDH will be repaired. The pediatric surgeons at Primary Children’s Hospital have expertise in all options of repair, including: an open or thoracoscopic approach; primary, patch, or muscle flap repair. The pediatric surgeon will discuss all of these surgical options in detail with you prior to the procedure and help determine which repair option is best for your child. The median age at repair is 3.7 days old and 75% of children treated here are repaired by the 6th day of life.

Once the repair is completed, care for your child still remains a drawn out process. Time is required in order to slowly turn down the breathing machine as well as other medications that support life. It also takes time to start feedings and to get to the point where enough nutrition can being given to go home. Approximately 10 – 15% of children will require an additional procedure prior to discharge. You should anticipate a prolonged hospital course: even a mild severity child spends an average to 4 – 8 weeks in the NICU, with an anticipated average stay of 4 – 6 months for severe and very severe children.
Our Outcomes at Primary Children's Hospital

Utah CDH outcomes 2003 - 2024
We participate in data collection with both the Children's Hospital Association (CHA) and the CDH Study Group (CDHSG). In 2016, we changed out management of these kids, which has significantly increased survival in those with and without ECMO, as well as significantly decreased our overall utilization of ECMO. This trend has continued through 2024.

Published Utah outcomes compared to other published studies
We have also published many studies demonstrating our outcomes, which are not only better than previously published studies, but well above the national averages in both the CHA and CDHSG datasets.

Utah outcomes in SEVERE CDH (MRI O/E < 25%) compared to FETO
Utah outcomes in SEVERE CDH (MRI O/E < 25%) compared to FETO
Utah outcomes in SEVERE CDH (MRI O/E < 25%) compared to FETO
Compared to published results in 2021 of the TOTAL trial (Deprest J et al. NEMJ 2021), our outcomes for children with severe CDH (MRI O/E < 25%) are significantly better than those that underwent FETO in the TOTAL Trial.
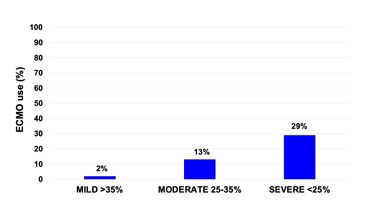
Need for ECMO in Utah based on severity of CDH
Utah outcomes in SEVERE CDH (MRI O/E < 25%) compared to FETO
Utah outcomes in SEVERE CDH (MRI O/E < 25%) compared to FETO
Since changing to our unique protocol of care in 2016, we have dramatically decreased the need for ECMO in children we treat with CDH. We have full ECMO capabilities, however, use it judiciously as there are known long-term consequences in children who have required it's support.
Our Pulmonary Hypoplasia Program offers Long-term support

What to expect after discharge from the hospital
Even with a mild CDH, once children leave the hospital, they will need long-term follow-up and support. We have a specialized multidisciplinary care clinic at Primary Children's Hospital for kids born with pulmonary hypoplasia (CDH, large CLM, giant omphalocele, PPH) called the Pulmonary Hypoplasia Program (PHP). Your child will follow-up frequently in this clinic and meet with multiple specialists who are experts in the care of CDH and will make sure they are growing and developing normally.
These specialists include:
- Pediatric Cardiologist
- Pediatric Pulmonologist
- Pediatric Surgeon
- Pediatric Neurologist
- Developmental Pediatrician
- Occupational therapist
- Physical therapist
- Speech therapist
- Dietician
(pic: one of our patients with severe CDH who is now home)
We are active in researching how to improve the care of kids
Follow the link below to see studies on CDH from our specialists who care for these complicated kids
Our Partners




Copyright © 2025 Grant Scott Bonham Fetal Center - All Rights Reserved.
Phone: (801) 662-6474
Fax: (801) 442-0570
info@grantscottbonhamfetalcenter.org