Understanding gastroschisis

What is gastroschisis?
Gastroschisis is a condition where a baby is born with an opening in the abdominal wall, at the umbilicus (belly button), most often to the right of the umbilical cord allowing some of their belly organs (like intestines) to stick out without a covering into the amniotic fluid.
- Occurs in about 3-5 in 10,000 live births
- The organs are NOT covered by a protective sac, unlike omphalocele where a sac is present
- The amniotic fluid causes inflammation to occur in the organs which can lead to thickening and dysfunction
- Rarely occurs along with other conditions, such as heart problems or chromosome differences
- At some point the baby will need surgery to put the organs back inside and close the belly

Fetal Center: the first step in gastroschisis care
Multidisciplinary Evaluation: meet with MFM specialist, pediatric surgeon, neonatologist, and other experts who will care for your baby
Comprehensive Imaging: detailed ultrasounds and other tests when indicated to assess your baby's condition and help plan treatment
Coordinated Delivery Planning: our team works to ensure your baby receives immediate specialized care at birth
How is gastroschisis evaluated?
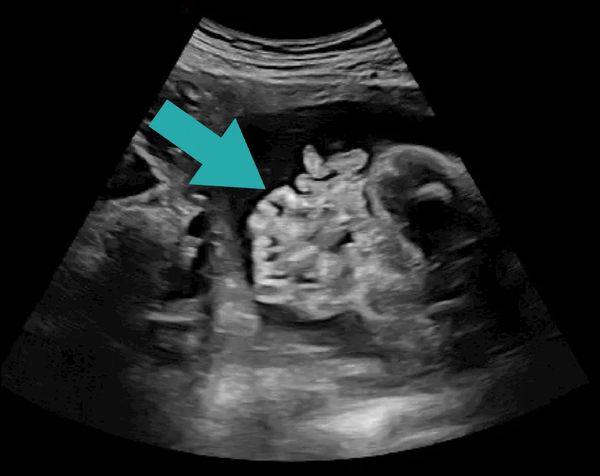
- Regular monitoring with a detailed ultrasound throughout pregnancy is recommended to track changes
- A fetal MRI in not obtained routinely, but sometimes when indicated to further evaluate other structures as indicated
- Genetic testing is not typically recommended as it is usually isolated without chromosomal abnormalities
(Pic: fetal ultrasound with arrow demonstrating gastroschisis)

When should the baby deliver?
Babies with gastroschisis are smaller and typically deliver earlier than those without. A normal vaginal delivery can occur, and a cesarean section is usually only required for common indications, not the gastroschisis. These babies benefit from planned delivery at a center with neonatal intensive care and pediatric surgery. We help schedule the delivery of all our mothers whose baby has a diagnosis of gastroschisis
The optimal timing of delivery is not known. Some believe it may be better to delivery early, whereas others later. We are currently participating in the Gastroschisis Outcomes of Delivery (GOOD) study to help understand the best timing for delivery. We discuss all delivery options in detail with our patients
What is the initial treatment?
The first step in management is neonatal resuscitation and stabilization, making sure the baby is able to breathe appropriately and the heart is functioning properly. A oral gastric tube is also placed in the mouth down into the stomach to remove any liquids
A special IV is placed called a PICC line which will allow for laboratory evaluation, as well as giving fluids and nutrition
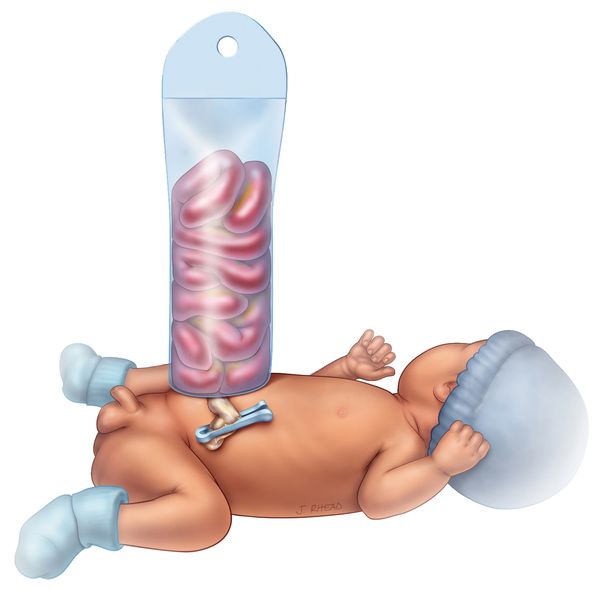
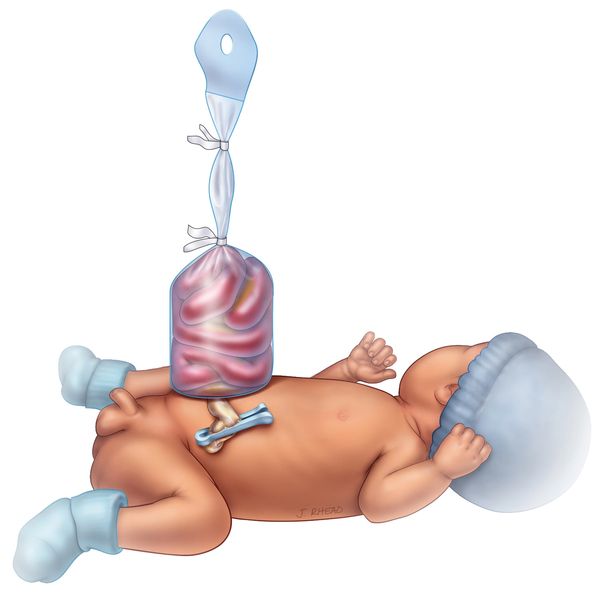
The gastroschisis is evaluated by the surgical team and placed into a silastic silo to help protect and allow for the abdominal organs to fall gently into the abdomen
Gastroschisis reduction
Over the next several days, the surgical team will slowly apply pressure to the silo helping the abdominal organs completely reduce into the abdominal cavity
Surgical closure
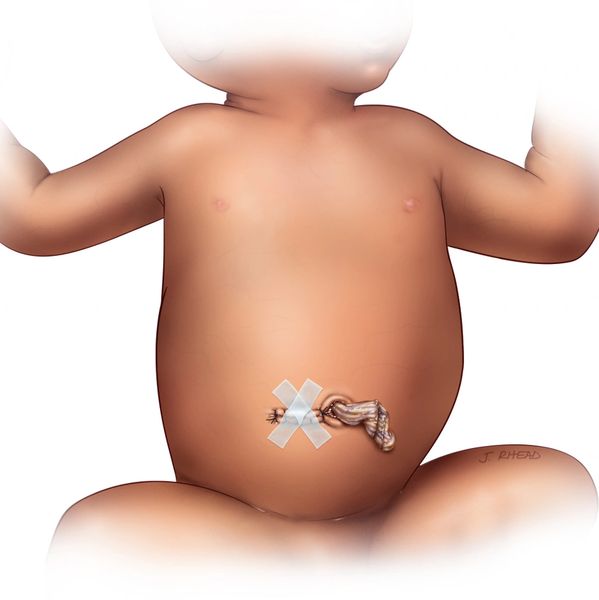
Once the gastroschisis is completely reduced, the opening can be closed. This can be done in a couple of different ways:
Sutureless closure: this occurs in a smaller portion of kids in the right condition, where the umbilical cord stump is used to close the defect and a dressing is applied. The dressing usually stays in place for a week. This typically results in an umbilical hernia, which may decrease and go away in time. Some kids may require surgery to fix the hernia later in life.
Primary closure: more often, the child will be taken to the operating room where the muscle and skin are closed by surgery. In some cases, the umbilical cord stump remain and fall off as usual. Most will result in a scar that looks like a belly button.

Neonatal care
Babies with gastroschisis are cared for in the Neonatal Intensive Care Unit (NICU). Feeding by mouth or tube is delayed until the abdominal organs are in the abdomen and the intestines recover and start working. Until then, IV nutrition (TPN) is given, often for weeks. The overall, Length of stay varies, but averages 6 - 8 weeks for uncomplicated cases, which occurs 75 - 80%
Complicated gastroschisis occurs in 15 - 20% of cases, which can result in the need for multiple operations and prolonged hospital course. Complicated gastroschisis includes:
- Partial closure or fusion of the skin to the gastroschisis making it difficult to place a silo and/or reduce the abdominal organs back into the abdomen
- Perforation of the intestine
- Intestinal atresia which is a blockage or missing part of the intestinte
- Loss of a significant amount of intestine, resulting in short gut syndrome, or not having enough intestine to absorb proper nutrients when eating

Outcomes and Long-term outlook
Most babies with gastroschisis do very well and grow up healthy. Long-term problems are uncommon, especially with those with uncomplicated gastroschisis
Children with complicated gastroschisis may experience feeding difficulties early on with slow bowel function that may lead to longer hospital stays
These babies require close follow-up with pediatric surgery and their primary care provider upon discharge for growth, nutrition, and bowel function. Most children do not have lasting physical limitations
(Pic: Dr. Fenton seeing a patient in clinic)
Our Partners




Copyright © 2025 Grant Scott Bonham Fetal Center - All Rights Reserved.
Phone: (801) 662-6474
Fax: (801) 442-0570
info@grantscottbonhamfetalcenter.org